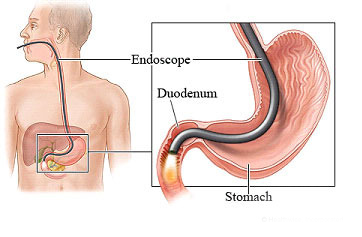
Upper endoscopy allows for examination of the lining of the upper part of the gastrointestinal (GI) tract, which includes the esophagus, stomach and duodenum (first portion of the small intestine). In upper endoscopy, the physician uses a thin, flexible tube called an endoscope. The endoscope has a lens and light source, which projects images on a video monitor. This procedure is also referred to as upper GI endoscopy, or esophagogastroduodenoscopy (EGD).
Upper endoscopy is often done under sedation to assure maximal patient comfort. Upper endoscopy helps the doctor evaluate symptoms of persistent upper abdominal pain, nausea, vomiting or difficulty swallowing. It is the best test for finding the cause of bleeding from the upper GI tract and is also more accurate than X-rays for detecting inflammation, ulcers and tumors of the esophagus, stomach, and duodenum. A physician may also use upper endoscopy to obtain small tissue samples (biopsies). A biopsy helps distinguish between benign and malignant (cancerous) tissues. Biopsies are taken for many reasons, and a doctor might order a biopsy even if cancer is not suspected. For example, a biopsy can be taken to test for Helicobacter pylori, a bacterium that can cause ulcers and celiac disease, an inflammatory condition of the small bowel that can lead to anaemia, weight loss and diarrhoea.
An upper endoscopy can also be used to perform a cytology (cell) test, in which a small brush is passed through the channel of the endoscope to collect cells for analysis. Other instruments can be passed through the endoscope to directly treat many abnormalities with little or no discomfort. For example, the doctor may stretch a narrow area (a stricture), detect Barrett’s esophagus (a possibly precancerous alteration in the esophageal lining), detect and biopsy gastrointestinal cancers, remove polyps (usually benign growths), treat bleeding (with standard cautery or the newer argon plasma coagulation method), and detect and treat symptoms of gastroesophageal reflux disease (GERD).